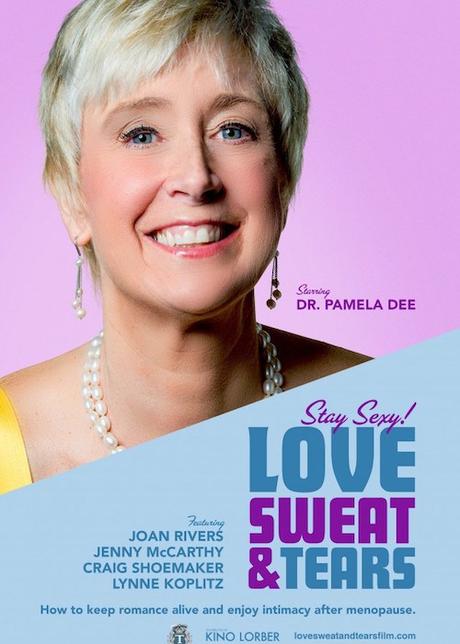
love, sweat, and tears
When I asked Dr. Pam Gaudry to share her personal story of how she came to create the film for menopausal women “Love, Sweat, and Tears”, I got way more than I bargained for. Her story brought me to tears at times.
Because she shares with such naked honesty her process of progressing from obstetrical physician to menopausal women’s advocate and then goes on to detail the tolls of caregiving, I am posting her poignant piece in two parts. More about “Love, Sweat, and Tears” at the end.
An Obstetrician’s Transition to Menopause and Survivorship Medicine
I fell in love with my job before I even had one. I delivered a baby. I brought life into the world. As a medical student, a wonderful couple let me into one of the most amazing and private events that they would ever have in their lives: the birth of their child. I was honored, thankful, appreciative, and overwhelmed. I could not believe that I could get paid for doing something so beautiful and miraculous. This first time and the last time that I delivered a baby, I was overwhelmed; I had butterflies in my stomach. I couldn’t wait to go to work every day of my life.
Why did your OB/GYN choose obstetrics and gynecology? Because pap smears are fun? Because we want to treat gonorrhea and chlamydia? Because it’s amazing to see a bladder falling out? No. They fell in love with the excitement of bringing a sweet, adorable new life into the world. Think about the fact that every time that an OB/GYN physician walks into an exam room with a pregnant woman, they have two patients in the room. An OB/GYN loves their patients, and they love being part of the family. They thrive on the excitement and thrill of bringing that life into the world. Obstetrics is our first love.
In 2005, I had a bustling obstetrics practice, my husband became ill with an oral cancer, I had 8-year-old twins, I was spending 6-8 nights a month in the hospital, and I was profoundly overwhelmed. Something had to give. Unfortunately, I had to give up the best part of my job – delivering my babies.
I really thought that I would hone my gynecologic surgical skills and become a better surgeon, and to some extent, that did happen. However, I was flabbergasted that women were coming in just to “talk.” I was shocked. The major comment that I got was that they were glad that I now had time to address their gynecologic issues. What? I had always addressed their gynecologic issues. How could they say that? Well, it became apparent that I did not. I especially did not address menopausal and intimacy issues. When I thought about it, I realized that I very superficially discussed menopause and did not touch on the ‘legion’ of problems that peri-menopause and menopause causes.
I was always (very happily) running to Labor and Delivery and (unhappily) trying to rectify being very behind schedule in the office. There is no way to be an obstetrician and, “plan your day” – let alone your schedule. When I had to stop delivering babies, my days changed overnight. When I did obstetrics, a normal day was running from room to room and then to Labor and Delivery and then back to the office where I (usually unsuccessfully) tried to catch up to the schedule. After I stopped doing obstetrics, I found myself entering a room, calmly sitting down, and talking to a patient for 20 minutes or so about menopausal and intimacy issues.
To be honest, I really did not have much training in this area; I went and got some. I decided to become a certified menopause practitioner through the North American Menopause Society. Additionally, I spent a couple of years getting a medical sex therapy certification. There are not many gynecologists that have this kind of training. Patients probably think that it is inherently part of our residency training in obstetrics and gynecology. Unbelievably, it is not. There is no information or training to draw from when treating these patients. An OB/GYN must rely on their own personal experience as well as the experiences that we encounter during years of practice. Surprisingly, in 2017, only 20% of residency programs have training in menopause and sexual medicine. Kind of frightening and sad, isn’t it?
So many women ask me why their OB/GYN had not given them information about the changes that occur in the peri-menopausal transition. My answer? They don’t know what they don’t know.
I had no idea that I was not really paying attention to my menopausal patients, and I’m sure that other OB/GYNs don’t know that either. But, think about it. If a physician rushes into the room, stands up the whole time, asks if you have any new problems or concerns, and you both know that the waiting room is full of pregnant women, crying babies, and strollers, and you know that there are probably two people in labor, it isn’t an atmosphere conducive to a discussion about your vaginal dryness, relationship issues (code word for sexual dysfunction and pain), hot flashes, and rage (pushing you to think about killing people).
When I look back, I feel badly about it; I (unknowingly) blew them off. I probably, and very nicely, told them to try some systemic estrogen – and, oh by the way – it can give you breast cancer and blood clots. After a quick exam, I was out the door. There are sweet wonderful babies to deliver; there are mamas to comfort and reassure. I gotta go.
I do things differently now. I come in the room in a calm fashion, say hello, and sit down – giving my patient my full attention. I spaced my visits out to 30 minutes. I grab their hands and ask how they are handling the changes that their bodies have gone through in the last year. It is not uncommon for someone to burst into tears. I know now. My dear patient, I will take care of these issues with you and for you. If you were my patient in those first 18 years of my practice and I blew off your gynecologic and menopausal issues…I’m sorry. I didn’t know what I didn’t know.
Pamela Dee Gaudry, MD, NCMP
NAMS Certified Menopause Practioner
Medical Sex Therapist
Survivorship Medicine Physician
(and I’m still an Obstetrician

You can host a screening at a theater near you of Dr. Pam’s film, “Love, Sweat, and Tears” through Gathr – they handle the details, it costs you nothing – you get your friends to go and promote the film. Click here for details.

