
Hyperinsulinemia plays the dominant role in provoking obesity and fatty liver disease, but what causes it?
Insulin is intimately related to our diet, so that was naturally the first place to look. Highly refined and processed carbohydrates, such as sugars, flour, bread, pasta, muffins, donuts, rice and potatoes are well known to raise blood glucose and insulin production. This became known as the carbohydrate-insulin hypothesis, and forms the rational basis for many of the low-carbohydrate diets such as the Atkins diet.
These are not new ideas, but very old ones. The first low carbohydrate diet dates all the way back to the mid 19th century. William Banting (1796-1878) published in 1863 the pamphlet Letter on Corpulence, Addressed to the Public, which is often considered the world's first diet book. Weighing 202 pounds (91.6 kilograms), Banting had been trying unsuccessfully to lose weight by eating less and exercising more. But, just as today's dieters, he was unsuccessful.
For all the success of low-carb diets, the carbohydrate insulin hypothesis remains incomplete. High dietary intake of refined carbohydrates is an important contributor to high insulin levels, but not the only contributor. There are many other significant influences. For this, we need to understand insulin resistance.
Insulin resistance - The major player
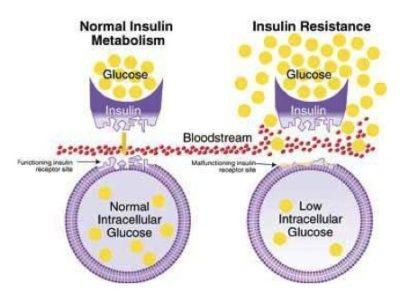
Insulin acts like a key to open a gate for glucose to enter the cell for energy. In the insulin resistance state, normal levels of insulin no longer open this gate and glucose piles up outside in the bloodstream.
Does obesity cause IR?
Type 2 diabetes is a disease of high insulin resistance. Obesity typically precedes the diagnosis of type 2 diabetes by a decade or more, so many presume that obesity itself causes insulin resistance. Decreased insulin resistance often accompanies weight loss. Insulin resistance gradually increases with obesity and further with pre-diabetes and type 2 diabetes. Obese, but otherwise normal (non-diabetic) patients have substantially increased insulin resistance compared to lean patients. Insulin resistance increases as you progress through the spectrum of obesity, pre-diabetes and then type 2 diabetes.
Understanding how obesity actually causes insulin resistance proved difficult. The first suspect was elevated fatty acids in the blood, which are increased with obesity. Insulin activates LPL, moving those fatty acids into adipocytes for storage. Fatty acid levels should not stay high unless insulin is not working properly. In other words, insulin resistance causes high fatty acid levels, rather than the other way around. This is reinforced by the fact that infusions of free fatty acids into the blood do not raise insulin resistance.
So, if fatty acids were not the causal factor, what was? Adiponectin, involved in fatty acid oxidation, was identified in 1995. However, the role it plays in obesity and IR is still unknown. Resistin, discovered in 2001, was given its name in the mistaken belief that it was the long-lost hormone that caused insulin resistance. Other factors such as interleukin-6, tumor necrosis factor, retinol-binding protein 4 and plasminogen-activating factor has all been investigated as a contributing hormone, but all have been found inadequate.
Unable to find the hormonal mediator of insulin resistance despite 35 years of intensive and dogged research, it is best to consider that perhaps obesity does not cause insulin resistance. After all, obesity and insulin resistance can be related in three possible ways. First, obesity might cause IR. However, this does not explain the importance of central obesity, or how type 2 diabetes can develop in normal weight patients. Insulin resistance may cause obesity, but this is unlikely since obesity typically pre-dates insulin resistance. Decades of intense research yields no definitive proof exists that either is true.
Metabolic syndrome
Our understanding of the metabolic syndrome began in the 1950s, when high triglycerides were noted to be highly associated with CV disease. In 1961, Dr. Ahrens showed that this abnormality was primarily related to excess dietary carbohydrates rather than dietary fat, as widely expected at the time.
Around the same time, early insulin assays confirmed that many people with relatively minor blood glucose elevations had severe hyperinsulinemia. This was understood as a compensatory mechanism to the elevated insulin resistance. In 1963, the observation that patients with heart attacks often had both high triglycerides and hyperinsulinemia first linked these two diseases.
High blood pressure (hypertension) was associated with hyperinsulinemia as early as 1966 (9). By 1985, researchers showed that much of essential hypertension, so called because the underlying cause had not been identified, was also closely associated with high insulin levels.
By the 1980s all the essential features of metabolic syndrome were identified and established - central obesity, insulin resistance, dyslipidemia (high triglycerides and low HDL) and hypertension. Dr. Gerald Reaven of Stanford University introduced this concept of a single syndrome in his Banting Medal address of 1988, one of the highest profile academic lectures in all of diabetic medicine, calling it 'Syndrome X'.
The 'X' moniker was chosen since it is commonly used in algebra to denote this single unknown variable, emphasizing that this syndrome shared a common underlying pathophysiology as yet unknown. These were not all individual risk factors, but one unified, critically important syndrome.
Criteria for metabolic syndrome
The 2005 National Cholesterol Education Program (NCEP) Adult Treatment Program III (ATP III) defines the metabolic syndrome as three of the following five conditions:
- Abdominal obesity - Men over 40 inches, women over 35 inches
- High Blood Glucose - over 100 mg/dL or taking medication
- High Triglycerides - > 150 mg/dL or taking medication
- Low High Density Lipoprotein (HDL) - <40 mg/dL (men) or <50 mg/dL (women) or taking medication
- High Blood pressure - >130 mmHg systolic or >85 diastolic or taking medications
Each additional component of metabolic syndrome increases the risk of future cardiovascular disease. The metabolic syndrome identifies patients with shared group of risk factors that all have a common origin. Insulin resistance, central obesity, high blood pressure and abnormal lipids all reflect a single underlying problem, the unknown X. While obesity is commonly associated, the metabolic syndrome could also be found in approximately 25% of non-obese individuals with normal glucose tolerance levels.
Why LDL is not a criterion
High levels of Low Density Lipoprotein (LDL or 'bad' cholesterol) are pointedly NOT one of the criterions of the metabolic syndrome. Many doctors and professional guidelines obsess about LDL, and resort to prescribing statin medications to lower it. High LDL is not part of constellation of the metabolic syndrome, and may not have the same origins.
The prevalence of metabolic syndrome in the United States varies from 22% to 34% depending upon the specific criteria. This is not a rare disease, but instead one that affects close to one third of the adult population of North America. This constellation increases the risk of heart disease by almost 300%. Metabolic syndrome also increased the risk of stroke, cancer, NASH, PCOS, and obstructive sleep apnea. Even more worrisome, this MetS is increasingly being diagnosed in children.
Recent research has supported and extended this concept of a single syndrome with a common cause. Other metabolic abnormalities, including endothelial dysfunction, increased inflammation, sympathetic tone and coagulation have been noted. All the major diseases of the 21st century were all related to a common cause. But what was it?
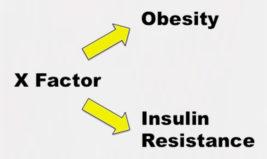
Dr. Reaven hypothesized that chronically hyperinsulinemia was not so innocent. Hyperinsulinemia may cause hypertension through salt and water retention. Hyperinsulinemia stimulates triglyceride synthesis in the liver, which are secreted into the bloodstream as VLDL. Hyperinsulinemia causes obesity. Hyperinsulinemia was causing insulin resistance.
-
Jason Fung

