 source: unfortunately don’t know but I love this painting
source: unfortunately don’t know but I love this painting
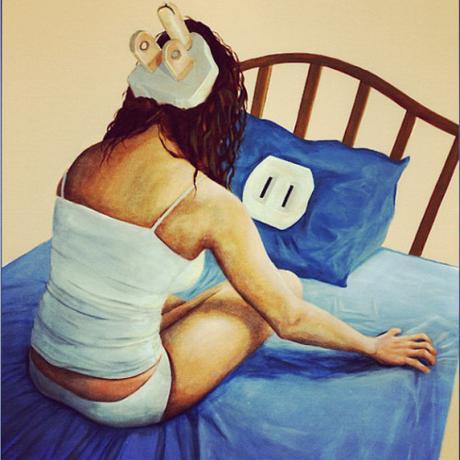
When I first sleep with someone we have to have the talk. “You really wear one of those?” she’ll ask. “Yeah, and I like to put these in too. And if you could, I’d prefer it if you don’t touch me at all.”
It’s embarrassing to sleep with an eye mask and earplugs, but what am I suppose to do? I’m bad at sleeping. People usually laugh at me when I say that, but it’s true. I think there are two types of people in the world—those who are bad at sleeping and those who are bad at staying awake, and I would make a badass night watchman.
Sleep is important, not just for feeling awake during the day and brain health, but also for the regulation of stress, inflammation, and the immune system, so disruptions to sleep increase the risk of not just mental illnesses like depression, but also infectious diseases, heart disease, and cancer.
 Modified version of Alex Gray’s Insomnia
Modified version of Alex Gray’s Insomnia
Growing Up In Insomnia
Insomnia is a place, a surreal, solitary, silent world I find myself in while the rest of the world slept. I’ve been visiting it as long as I can remember, but only recently have I come to terms with it. It’s the bedroom ceiling, the green trapezoid display of a digital clock.
Sometimes, I’d lie in bed, feeling exhaustion behind my eyes, as if my heart had grabbed onto my optic nerves, and was trying to pull my eyeballs down into my chest, but I’d simultaneously know my thoughts tumbling, they wouldn’t slow down anytime soon, and I’d realize I was stuck in insomnia. Other times, even before getting in bed, I would just feel simply awake, as if my body unaware it was the middle of the night and not the middle of the day, and I’d know I was there.
Long before my high school days of sneaking out of the house, I had already learned which squeaky steps I needed to skip over to avoid waking my parents. I’d creep downstairs, microwave a glass of milk, and hunker down in front of late-night infomercial hell.
By high school I was dabbling in drugs, and I’d keep a stash in my bedroom. I’d buy them from the local drugstore: melatonin, valerian root—Oh God! I can remember the heartburn and awful herbal taste of valerian root burps. I’d normally only bust out my drugs on special occasions, nights I knew I wouldn’t be getting much sleep–before the first day of school, a cross-country race, or going camping. It wasn’t even necessarily events I was nervous or even excited about. The anticipation of novelty is enough to keep me up.
College presented it’s own set of problems—parties next door, people yelling in the hallway, and a freshman roommate with a penchant for getting up early, eating a bowl of cereal, and dragging his metal spoon along the edges of his porcelain bowl to get every last flake. I started wearing earplugs.

A Cup of Ambition
College is also where I discovered the drug that’s a godsend for an insomniac—coffee. What? I can actually focus in a 9am class? But it’s a god-sent double-edged sword. Too much and I’ll be up all night in an over-caffeinated limbo: too wired to sleep, but too tired to do anything.
I since found out my body breaks down caffeine more slowly than most. When I analyzed some of my DNA through 23&Me, I learned that I’m a homozygous caffeine slow metabolizer.

That means I have to copies of the ‘C’ genetic variant affecting my liver enzyme, CYP1A2, which breaks down caffeine (and many other substances), and means my versions of this enzyme likely works slower than 85% of people’s. As of 2013, the story is a bit complicated. It appears, that my variant of this enzyme may work at similar speeds in baseline conditions, but it’s activity isn’t increased as much through daily coffee consumption. So for people with either variant who have never drunk caffeine, their response to caffeine will be similar. But when most people drink coffee daily, those with the ‘A’ allele, they will quickly become ‘metabolically’ or ‘pharmokinetically’ tolerant to it because their liver is breaking down more of the caffeine before it reaches the brain. However, people like me with the ‘C’ allele enzyme won’t develop as much of this metabolic tolerance. People like me with two ‘C’s are more likely to get heart attacks if we drink a few coffees a day than people with the ‘A’ allele, but on the bright side we’re cheap coffee dates?
Maybe because of my underlying insomnia, or my slow caffeine metabolism but I’ve always envious of people who can drink a coffee at night and then fall asleep. “I’m addicted to coffee,” these people often say.
Tangent – is caffeine addictive?
It’s controversial whether coffee is addictive, but I have a strong opinion. People can definitely build a strong tolerance to it and maybe experience withdrawal symptoms like a headache in the morning if they don’t drink it. Therefore, you might say they’ve grown physical dependent and tolerant to caffeine, but I wouldn’t say their addicted. Keep in mind that same thing occurs with people taking heart medication. People may need to up your dose over time to keep their heart rate low (tolerance), and if they suddenly stop taking that medicine, their heart rate will speed up to the extent it could even cause a heart attack or kill them (withdrawal).
However, I don’t think it makes sense to say these people are addicted to their heart medication. No one is getting their kicks off of heart medication, but many people, myself included, love their coffee. One of caffeine’s molecular targets is an adenosine receptor, which is highly enriched in the ventral tegmental area (VTA), an important component of the neural reward circuitry, which all addictive drugs target.
I once saw Eric Nestler—this guy literally wrote the textbook on how drugs affect the brain—give a talk on addiction and he brought up that he didn’t think caffeine was addictive according to the definition doctor’s use. The clinical definition of addiction is “a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences.” Nestler said he had never heard of people compulsively using caffeine despite harmful consequences.
Here, I’ll be bold enough to disagree with the textbook-writing superstar scholar. For a year in medical school I shadowed a cardiology clinic, and met more than one little-old southern ladies, who refused to give up their coffee or even switch to decaf, despite their cardiologist telling them the caffeine was dangerous for their heart. They were so vehement about it, they wouldn’t even just lie to their doctor and drink it behind his back. “I need my coffee,” they’d say. That’s what a coffee addict looks like.
My Visit to the Sleep Doctor? The Pulmonologist?
In graduate school I finally visited a doctor about my sleep. Maybe because the stress of grad school was making it worse, or maybe because I had learned enough about the medical system to realize that if this was a problem that was bothering me, I had to take action myself and seek out care, and I finally wanted to take control of this part of my life. I was tired of worrying about sleeping the night before the exam more than worrying about the exam itself, and yawning through what should have been the most exciting days of my life.
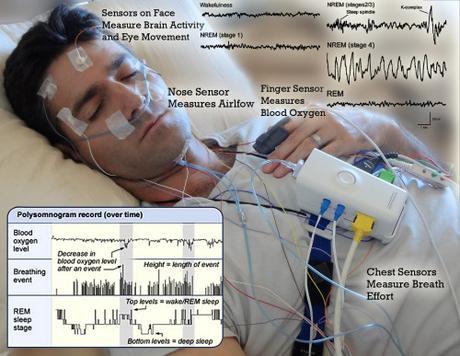
But the real reason I had probably put of going to a sleep doctor was that I worried it would shatter a long-running fantasy. In my imagination, I would go and the doctor and describe my sleep problems, and he or she would listen, concerned, and tell me to come back for a sleep study. In the hospital laboratory, my head covered in electrodes and wires, I would of course struggle to fall asleep, and my brain would generate signals pathognomonic for, or highly indicative of some treatable disease. After treatment my sleep problems would go away, that mental fogginess that sometimes makes it difficult to think clearly would disappear—the feelings I had mistaken for laziness were really just symptoms of my disease, and far from lazy I would become the prolific, productive person I want to be.
So yeah, you could say I went in to my appointment with unreasonable expectations.
It was actually kind of a crazy. The doctor I was referred to I had met before. He had lectured me in med school, and rumor had it he was the son of the real life Doc Hollywood (he has the same name but Wikipedia says otherwise).
But, that’s not even the crazy part. What’s crazy is my sleep doctor was a pulmonologist—that’s right a lung doctor. Not a brain doctor, a lung doctor.
Actually it turns out it’s quite common for pulmonologists to become sleep specialists, because one of the most common sleep problems in the United States, where obesity is rampant, is sleep apnea. Sleep apneas is a disease where breathing halts in the middle of the night and disrupts sleep. Often patients suffering from sleep apnea are unaware of the problem unless a partner witnesses them gasping for breath in the middle of the night. (If you snore in the night and experience excessive daytime sleepiness, you should probably get yourself checked out.) Because pulmonologists are well trained in breathing-conditions, they can get certified as sleep specialists in half the time of other medical specialists like psychiatrists and neurologists.
The Appointment
After filling out a survey about my normal sleep experiences, I met with the doctor, and I learned my situation is pretty normal. Lot’s of people deal with insomnia and there’s little we can do about it. One sleepless night per month is in the range of normal the doctor told me, and he was a bit concerned I was reporting two a month on average.
I have a lot of difficulty falling asleep at night, but usually then will really struggle with getting up in the morning and excessive daytime sleepiness, which I learned were signs of a delayed or abnormally long circadian rhythm. Because of this altered circadian rhythm, I should take special avoid drinking coffee past noon and blue light after dark that disrupts your circadian rhythm, as your brain mistakes it for daylight. He noted that while delayed circadian rhythms are correlated with higher IQs, they are also correlated with people doing worse in school and at their jobs.
Source: Luke Mastin
Circadian Rhythm Aside
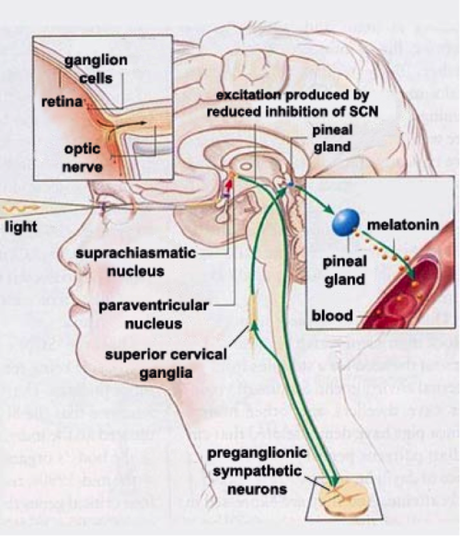
Most of life maintains a 24-hour or circadian rhythm: animals, plants, fungi, and even some bacteria do. The entire human body maintains a circadian rhythm, or 24-hour clock, which presents a problem—how do cells stay aligned with one another and the day night cycle? In charge of keeping the entire body in time with itself and the world is the Suprachiasmatic Nucleus (SCN)[1], a brain area in the hypothalamus. The SCN receives direct projections from a specialized photodetector in the retina which is sensitive to blue light—the intrinsically photosensitive Retinal Ganglia Cell (ipRGC)
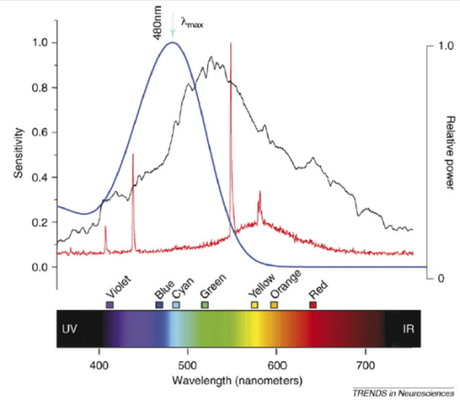
Blue: Action spectroscopy shows the melonopsin photopigment contained in retinal ganglion photodetectors is maximally sensitive to 480nm blue light, somewhat sensitive to green light and violet light, but largely unaffected by yellow, orange, and red light.
Black and Red: Comparisons of the spectrum admitted by traditional incandescent lightbulbs (black) and fluorescent light bulbs (red). Not these graphs are all normalized to the wavelength with the maximum intensity set to one.
Source: Hankins, et al. 2007.
Source: http://thebrain.mcgill.ca/flash/a/a_11/a_11_cr/a_11_cr_hor/a_11_cr_hor.html
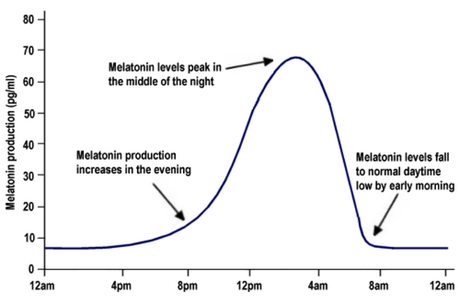
The blue light signals detected by the ipRGCs are converted into electric signals, and transmitted directly to the SCN. The SCN contains inhibitory neurons which project to another region of the hypothalamus, the periventricular nucleus. So in the presence of blue lights the SCN will be activated and inhibit the Paraventricular nucleus, blocking it’s signaling. In the absence of blue light, when the SCN is not activated, the paraventricular nucleus signals down actually to sympathetic neurons in the spinal cord, which signal back up throught the superior cervical ganglia back into the brain, where they stimulate the pineal gland to release melatonin into the bloodstream.
I’d already been trying to cut down on the blue light at night, using F.lux, and Twilight for my android phone to try to cut down on blue light at night. I’d even gone so far as to buy glasses that filter out blue light. (They’re actually really fun to mess around with, so I ended up buying a bunch of different colors for fun–I’m a nerd, don’t judge me. There are also hip versions, if you want to go out with them, and don’t want to look like a mad scientist, but still be that dude wearing sunglasses at night.)
For me, the doctor also recommended taking melatonin every night. While in high school I had taken it to help with days I felt sleep was particularly important and I was unlikely to get it, the doctor told me it’s more effective when it’s taken daily and consistently. Instead of thinking about it as a sleep inducer, it’s better to think more as a way to shift and normalize your circadian rhythm over time. Similarly, he recommended using a light box in the morning or trying to get some sunlight early. (I wonder if my eye-mask is delaying the light signals in the morning and actually a bit counter-productive.)
On especially tough nights he recommended taking Benadryl, or diphenhydramine, for it’s drowsy side-effects (unlike non-drowsy anti-histamines, it easily crosses into the brain from the blood stream where it can block histamine receptors. Interestingly, histamine releasing neurons are the neurons in the brain that correlate the most with wakefulness.)
Using these drugs cold potentially cause dependency, but they are not thought to be addictive. (These are concepts I discussed above in the tangent about caffeine and addiction.) I did worry that potentially taking melatonin chronically could diminish my pineal’s ability to naturally produce it. This phenomenon is seen with other hormones, for example why taking anabolic steroids can shrink the testicles. While the doctor couldn’t speak to that specifically, he said he had patients who had been taking it for decades and none of them had ever complained about side effects. Essentially, yeah, maybe you’ll have to take it for the rest of your life, but it’s over the counter, cheap, with few known side effects. There are some side effects including headaches, depression, and ironically daytime sleepiness. Hopefully this goes without saying, but you should talk with your doctor before starting any new drug or supplement.
More generally, the evidence shows that for people suffering from insomnia, first doctors should check for another condition which may be exacerbating the problem: psychiatric illness, substance abuse, a specific sleep disorder, or side effect of a medical condition. Patients should practice proper sleep hygiene: try to sleep and wake at consistent times; avoid doing work in their bedroom; if in bed for more than 30 minutes without sleep, get up and do something until you feel tired; avoid bright lights, exercise, meals, nicotine or caffeine shortly before bed; try to control stress and practice intentional relaxation; try to exercise regularly; avoid daytime naps longer than 20-30 minutes. Further behavioral interventions like Congitive Behavioral Therapy for Insomnia and Sleep Restriction Therapy have also been shown to be effective. A number of drugs have been shown to be effective, though excluding melatonin these are normally only prescribed in extreme cases. These drugs include certain classes of anti-depressants, sedatives, and the newly FDA-approved orexin antagonists.

Conclusions
Going to the doctor didn’t give me any magic bullets, didn’t unlock any super-human abilities, but I think it has helped a bit. I go through phases where I sleep pretty normally, and others where it seems a nightly problem, maybe because of the twisted joke of psychogenic insomnia, essentially where worries about not sleeping make it harder for your brain to transition into sleep.
For me, the most effective way to get to sleep actually goes against many doctors’ recommendations not to do anything in your bed other than sleep. For me the most effective way to get to sleep is actually my mom’s perennial advice, and the habit I had as a child of reading to fall to sleep.
I’ll read and gradually turn down the knob on my halogen lamp, and when I notice I’ve lost my place on the page, or find myself blinking my eyes to stay awake, that’s when I lay the book down,
twist the light all the way off,
pull the eye-mask down over my eyes, the sheet up to my neck,
and I visit a world infinitely more pleasurable than insomnia—sleep.
———–
[1] The Suprachiasmatic Nucleus jargon broken down: It’s an area of the brain (or nucleus—different meaning of nucleus from the one where DNA is stored, fucking biologists) that lies on top of (or supra) the optic chiasm (chiasmatic), which is another part of the brain where the two optic nerves cross over one another and for an x-shape (like the greek letter chi).
———–
If you liked this article, please share or follow the blog to see more like it. I do this to share my love of neuroscience and psychology and also because of an insatiable need for the approval of strangers, so help me out!